
Dr Lau Kah Liew, clinical oncologist at the Borneo Medical Centre, Kuching and Malaysian Oncological Society committee member.
LIVING in a modest society, we tend to avoid talking about our private bodily functions as much as possible because it’s traditionally viewed as an uncouth and embarrassing subject.
In particular, anything that has to do with our bowels and their movements will usually leave a few of us cringing with embarrassment and begging to change the subject.
However, the health of our bowels — colon and rectum in particular — is an important topic that all of us will need to broach from time to time as the risk of developing colorectal cancer is a very real thing.
Coming in at our second most common cancer in Malaysia and Sarawak, colorectal cancer is a type of cancer that starts in our colon or rectum and has an estimated incidence rate per 100,000 of 14.6 and 11.1 for Malaysian males and females respectively.
Derived from the Malaysian National Cancer Registry Report 2007-2011, these figures indicate that the disease is the most common cancer found locally in males and the second most common cancer in females.
And global cancer rates are also reflecting this trend as colorectal cancer remains as our top three cancers.
But despite the disease’s position as such a commonly seen cancer, the Report also indicates that the percentage of colorectal cancer cases, detected at Stages I and II, is only 34.1 and 34.8 per cent for males and females respectively.
Explaining these disparaging rates, Dr Lau Kah Liew, a clinical oncologist and Malaysian Oncological Society (MOS) committee member, says this is due to a combination of low awareness of the disease, its characteristics as well as its difficult to detect nature.
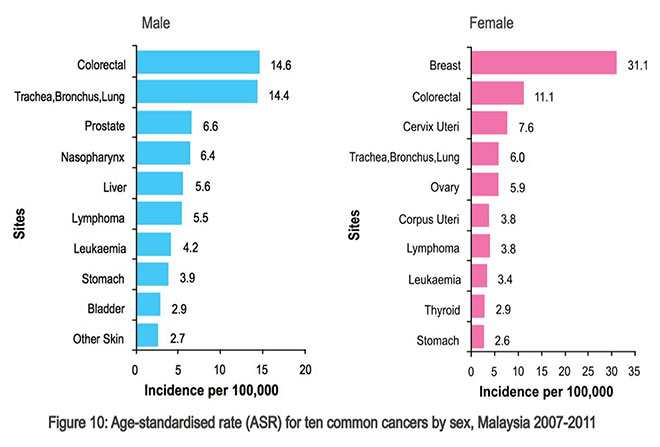
Incidence rates of top cancer types in Malaysia for males and females from 2007-2011.
Symptoms of Colorectal Cancer
According to Dr Lau, the non-specificity of its symptoms is the main reason why colorectal cancer and cancer in general is not easy to detect.
The common symptoms of colorectal cancer are changes in bowel habits such as the onset of diarrhea, constipation, narrowing of the stool, rectal bleeding, mucus discharge, persistent blood in stools and lower abdominal pain, bloating or discomfort.
“It is very hard to determine whether or not one of these symptoms is actually a result of the cancer because symptoms like lower abdominal pain, bloating and discomfort can easily be caused by slight changes in eating habits.
“Even other symptoms like rectal bleeding and bloody stools can seem normal for many people as they will just think that it’s caused by their hemorrhoids.
“These symptoms are all very non-specific and can mimic the symptoms of some very common gastrointestinal illnesses,” he explains.
Adding to that, detection is complicated as Dr Lau guides that the disease can also strike without any symptoms at all in its earlier stages.
So in the face of this camouflaged and sometimes silent disease, how exactly do we help promote earlier detection in our communities?
To this, Dr Lau recommends we can begin by placing more trust in our healthcare professionals and seek their advice whenever we experience something out of the norm.
“For example, if you notice any changes in your normal bowel habits with little change to your daily habits, I would suggest you come in for a further check just to be safe,” he advises.
And beyond just being more active in reporting our ill health and seeking medical care, Dr Lau also guides that there are some lifestyle-related factors we can modify to help reduce our risk of developing the disease.

The 10 most common cancers in Malaysia 2007-2011. Sources: Malaysian National Cancer Registry.
Risk factors
For colorectal cancer in particular, Dr Lau notes that links between the cancer and diet, weight and exercise are some of the strongest — for any type of cancer for that matter — further emphasising the importance of leading a healthy and active lifestyle.
“The risk of developing and dying from colorectal cancer is higher if you are overweight or obese and this is further amplified by a heightened risk from physical inactivity, so the more active you are, the better.
“As for diets, the ones high in red and processed meats and low in fibres can raise your risk of developing colorectal cancer.
“In addition, cooking meats at high temperatures like drying, broiling and grilling may also create chemicals that might raise your cancer risk.
“So I would recommend consuming these foods in moderation.”
Not forgetting the usual cancer-causing suspects — smoking and heavy alcohol use — Dr Lau strongly warns against picking up smoking or continuing the habit as smoking could easily increase the risk of us developing colorectal cancer by as much as 20 per cent.
“The disease has also been linked to heavy alcohol use, so limiting alcoholic drinks to no more than two a day for men and one a day for women could help lower the risk of colorectal cancer,” he adds.

Colorectal cancer is a type of cancer that starts in the colon or rectum.
Screening process
While embracing a healthier lifestyle can definitely help us lower our risk of developing colorectal cancer, it is also important to remember there are also risk factors beyond our control like being older and having a personal or family history of colorectal polyps or inflammatory bowel disease, an inherited syndrome for the cancer and Type Two diabetes.
Individuals fitting into these aforementioned categories all have a heightened risk of developing the cancer and it is recommended that they adopt different screening processes of the disease from the general populace.
But what exactly is the recommended screening process for colorectal cancer? And what should high risk individuals do differently?
Unfortunately, there is no one recommended screening process as there are a multitude of guidelines out in the world which all recommend different things.
Some countries offer screening through fecal occult blood tests (FOBT) biennially to detect blood in the stool while others recommend colonoscopies every 10 years to detect any abnormal growths.
The one thing they have in common, however, is that these tests are usually only offered to older individuals as colorectal cancer is much more common over the age of 60.
So for higher risk individuals, Dr Lau guides that it would really be up to their respective doctors to advise what screening process to adopt but it would likely involve screening at an earlier age or with increased frequencies.
However in saying this, he points out that all of these screening tests are not 100 per cent accurate as they may be easily affected by false positives or negatives.
In particular, the carcinoembryonic antigen (CEA) test or the tumour marker test, routinely offered in many blood testing packages, may show false positives as CEA levels may be increased in certain types of non-cancerous conditions.
“Some cancer patients have normal CEA levels whereas some healthy individuals have raised levels, and smokers who do not have cancer can also have an increased CEA values,” he reveals.
Due to these potential false results, Dr Lau counsels patients to not fret too much about the initial results of certain screening tests as more often than not, more than one test may be necessary to confirm or exclude a diagnosis of colorectal cancer.
Attitudes and treatments
But even if the patient has been diagnosed with the cancer, Dr Lau believes the best move will be to still remain calm because nothing in life is set in stone and each patient’s situation and outcome will differ from one another.
“When you are diagnosed with colorectal cancer or other types of cancers, don’t stress over survival rates because they are just estimates for how likely your treatment will be successful and won’t actually predict what will happen in any individual’s case.
“Instead, the best thing to do is to remain calm and gain a better understanding about your treatment options because now is the golden opportunity to begin treatment and take control of the disease because a disease is cured only when the patient is willing to overcome it.
“A doctor only helps the patient fight his or her illness.
It’s the patients themselves who fight their disease,” he shares.
For colorectal cancer, surgery is usually the main treatment in cases where the cancer is only found in one part of the body; it may be used alone or along with other treatments like chemotherapy or radiation therapy.
These treatments may be given before surgery to first shrink the tumour or after surgery to help reduce the risk of the cancer recurring.
During the first five years of a cancer going into remission, patients who has had the cancer involved with their lymph nodes will be at a higher risk of the cancer reoccurring, so often, chemotherapy in the form of a tablet or intravenous drip is given to patients to help manage this risk.
In addition, colonoscopies are also recommended one year after the primary treatment and if results are normal, once more in three years, then every five years.
Managed and not cured
While the idea of cancer recurring is a frightening thought for many cancer survivors, Dr Lau offers a different perspective.
“For me, I see cancer as a chronic disease like hypertension, diabetes and heart disease. And just like those diseases, cancer is to be managed and not cured.
“It’s definitely not a death sentence but just one type of illness and rather than fixate on whether it will come back or not, we should instead focus on achieving our own personal happiness.
“No matter how healthy or wealthy we are, we are all given 24 hours a day. So live every day to the fullest.”
About Dr Lau Kah Liew
- Since graduating from medical school in 2001, Dr Lau has had the opportunity to serve in various departments all over Malaysia.
- However he finally settled on the field on oncology and after finishing his specialist training in 2010, returned to Sarawak in 2013 to serve as the resident clinical oncologist at the Borneo Medical Centre.
- On why he has chosen to be an oncologist, he says: “If I can help a patient accept his or her cancer diagnosis, it will be a very rewarding experience for me.
- “Because not everyone can accept the disease and once they are able to accept it, they will become more willing to participate with me in treating and managing their illness.”
